Imagine you’ve been recommended a significant dental procedure—a crown, a bridge, or maybe even an implant. You feel a mix of relief that a solution is in sight and a knot of anxiety about the cost. You think your insurance will cover it, but then your dental office mentions “pre-authorization.” Your mind races: What is that? Do I need it? How long does it take? Will it even be approved? This feeling of uncertainty is incredibly common, especially when it comes to major dental work in Ontario. With the introduction of new programs like the Canadian Dental Care Plan (CDCP) and the existing complexities of private insurance, understanding when and why your dental treatment needs a “heads up” from your insurer is more important than ever. Here at Viva Dental Orangeville, located at 287 Broadway, Orangeville, Ontario, our mission is to provide patient-centered care and make your dental journey as smooth and clear as possible. We understand that navigating dental insurance can feel like deciphering a secret code.
That’s why we’ve put together this comprehensive guide to demystify pre-authorizations for major dental work, helping you understand the process, set realistic expectations, and avoid unexpected financial surprises.
What’s the Big Deal About Dental Pre-Authorization?
Think of pre-authorization (sometimes called pre-determination or an estimate) as a heads-up you give your insurance company before undergoing significant dental treatment.
It’s essentially asking, “Hey, I’m planning this procedure; will you cover it, and if so, how much?”
Why is this “heads up” so important?
- Financial Clarity: It gives you a clear estimate of what your insurance will cover and what your out-of-pocket expenses might be, helping you budget confidently.
- Treatment Planning: Knowing your coverage helps you and your dentist plan the most appropriate and affordable treatment path.
- Avoiding Surprises: No one likes an unexpected bill. Pre-authorization helps prevent that “sticker shock” moment.
Pre-Authorization vs. Pre-Determination: What’s the Difference?
These terms are often used interchangeably, but there’s a subtle distinction that can impact your understanding:
- Pre-Determination (or Treatment Estimate): This is the more common term. It’s a request sent to your insurance provider to determine your estimated coverage for a proposed treatment plan. The insurer reviews the plan and sends back a response detailing what they expect to cover. It’s an estimate, not a guarantee of payment until the service is rendered.
- Pre-Authorization: This term is often used when the insurer requires explicit approval before certain procedures can be performed and paid for. This is particularly common with newer plans like the CDCP or for very complex/expensive treatments with private insurers. It signifies a higher level of scrutiny and a more binding approval if granted.
For the purpose of this guide, we’ll generally use “pre-authorization” to cover both concepts, as the core intent—getting insurer approval/an estimate before treatment—remains the same.
The key takeaway is: both aim to clarify your coverage upfront.
When Does Your Dental Work Need a “Heads Up” from Insurance?
Generally, pre-authorization is required for major dental work or extensive procedures that involve higher costs. These are typically treatments beyond routine check-ups, cleanings, and simple fillings.
Here’s a list of common treatments that often require pre-authorization from insurance providers in Ontario, including under the Canadian Dental Care Plan (CDCP):
- Crowns: A cap placed over a damaged tooth to restore its shape, size, strength, and appearance.
- Bridges: Used to bridge the gap created by one or more missing teeth, anchored to natural teeth or implants.
- Dental Implants: A surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, or denture.
- Partial and Complete Dentures: Removable appliances that replace missing teeth and surrounding tissues.
- Root Canal Treatment (especially on molars): While some basic root canals might not, complex cases or those on molars often trigger pre-authorization.
- Orthodontic Treatment: Braces or [Link: Invisalign in Orangeville] for straightening teeth.
- Oral Surgery: More extensive surgical procedures, beyond simple extractions.
- Sedation Dentistry: Deeper levels of sedation beyond nitrous oxide (laughing gas) may require pre-authorization due to associated costs and complexity.
Why are these specific procedures often flagged?
It comes down to cost, complexity, and clinical necessity. Insurance companies want to ensure that expensive procedures are truly needed and meet specific clinical criteria.
They also have “frequency limitations,” meaning they might only cover a certain number of certain procedures (e.g., one crown on the same tooth every 5-7 years).
Navigating Pre-Authorization with the Canadian Dental Care Plan (CDCP)
The Canadian Dental Care Plan (CDCP) has brought dental coverage to many Canadians who previously lacked it.
While it’s a fantastic step forward, it’s crucial to understand that the CDCP is not a free dental program, and pre-authorization plays a significant role in its operation.
The CDCP covers a range of essential services, but for many major procedures, pre-authorization is mandatory. According to official sources like Canada.ca, services requiring pre-authorization include:
- Crowns
- Bridges
- Dentures (partial and complete)
- Dental Implants
- More complex oral surgeries
- Root canal treatments on permanent molars
A Crucial Insight: Setting Realistic Expectations for CDCP Pre-Authorization
Recent reports, like those highlighted by CBC News, indicate that the CDCP pre-authorization process has faced “growing pains.”
Shockingly, over half (52%) of requests for complex dental work under the CDCP have been rejected or required more information since its launch.
This high denial rate isn’t necessarily a permanent “no” to your treatment, but it does mean:
- Delays are common: Submitting, waiting for a decision, potentially resubmitting, and waiting again can significantly extend treatment timelines.
- Documentation is critical: The CDCP requires very specific clinical documentation to justify treatment.
- Appeals are often necessary: Don’t be discouraged by an initial denial. It might simply mean more information is needed.
This makes understanding and proactively navigating the pre-authorization process even more vital for CDCP beneficiaries.
Your Step-by-Step Journey to Pre-Authorization Approval
While the specifics can vary slightly between private insurance providers and the CDCP, the general process is similar. Here’s a typical journey:

Step 1: Initial Consultation and Treatment Plan
Your journey begins with a thorough dental examination at our Orangeville office. Dr. Sahar Rakhshanfar and our team will assess your oral health, discuss your concerns, and recommend a personalized treatment plan.
For major procedures, this plan will detail the proposed work, estimated costs, and supporting clinical evidence.
Step 2: Gathering the Necessary Documentation
This is where your dental office truly shines. We will gather all the required information to support your pre-authorization request. This typically includes:
- Detailed Treatment Plan: Outlining each procedure, tooth numbers, and estimated fees.
- Diagnostic X-rays: Providing visual evidence of the dental condition.
- Clinical Notes and Photos: Detailed descriptions of the condition, prognosis, and why the proposed treatment is necessary and appropriate.
- Periodontal Charting: For procedures involving gum health, showing measurements and current condition.
- Any supporting specialist reports.
The quality and completeness of this documentation are paramount.
Insurers, especially the CDCP, are looking for clear justification that the treatment meets their clinical criteria.
Step 3: Submission by Your Dentist
Once all documentation is compiled, your dental office submits the pre-authorization request to your insurance provider.
This is usually done electronically (EDI) for speed and efficiency, though some cases might require submission by mail.
Step 4: The Waiting Game
After submission, there’s a waiting period while the insurance company reviews the request.
- For private insurance: This can range from a few days to a couple of weeks.
- For CDCP: Currently, wait times can be longer due to the volume of applications and the detailed review process. Setting realistic expectations for several weeks or even a month or more is advisable.
Our team at Viva Dental will keep you informed of any updates we receive.
Step 5: Receiving the Decision
Eventually, your dental office will receive a response from your insurance provider. The decision can be:
- Approved: Great news! The insurer outlines what they will cover, including your co-payment.
- Approved with Modifications: The insurer may approve a different, less expensive treatment alternative or cover only part of the proposed plan.
- Request for More Information: The insurer needs additional clinical details to make a decision. This is common with CDCP denials.
- Denied: The insurer determines the treatment is not covered or doesn’t meet their criteria.
What Happens If Your Pre-Authorization is Denied? Don’t Panic!
A denial isn’t necessarily the end of the road. With the high denial rates reported for CDCP, understanding your options is crucial.
Common Reasons for Denial:
- Incomplete/Insufficient Documentation: The most frequent culprit. The insurer simply didn’t have enough information to approve the claim.
- Does Not Meet Clinical Criteria: The proposed treatment might not align with the insurer’s specific guidelines for medical necessity or appropriateness (e.g., a tooth might not be deemed “restorable” enough for a crown).
- Frequency Limitations: You might have received a similar treatment too recently, according to your plan’s rules.
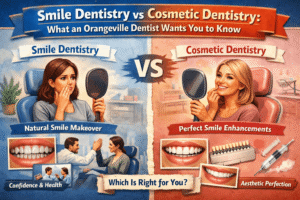
- Treatment is Deemed “Cosmetic”: Some procedures may be seen as purely cosmetic rather than functionally necessary by the insurer.
- Waiting Periods/Eligibility Issues: Your plan might have waiting periods before certain benefits kick in, or there could be an issue with your overall eligibility.
Your Options After a Denial:
- Gather More Information: Often, a denial is just a request for more details. Our team can review the denial reason and provide the additional X-rays, notes, or justification needed.
- Appeal the Decision: You have the right to appeal. This usually involves resubmitting the claim with more robust documentation and a letter explaining the necessity of the treatment. We will support you through this process.
- Consider Alternative Treatments: If the initially proposed treatment remains denied, your dentist can discuss alternative, potentially covered, treatment options.
- Understand Your Out-of-Pocket Costs: If an appeal is unsuccessful or you choose to proceed without full coverage, we will provide a clear breakdown of your financial responsibility.
At Viva Dental Orangeville, we leverage the latest dental technologies and our expertise to present the strongest possible case for your treatment needs, e.g., teeth whitening.
We believe in transparency and empowering you with the knowledge to make informed decisions about your oral health.
Beyond Pre-Authorization: Understanding Your Financial Piece of the Puzzle
Even with a pre-authorization approval, it’s important to understand your financial obligations.

- Co-payments: Most insurance plans, including CDCP (unless you have a very low adjusted family net income), require you to pay a percentage of the treatment cost. This is your “co-payment.”
- Balance Billing: If your dentist’s fees are higher than what your insurance plan will cover (the “fee guide” amount), you may be responsible for the difference, known as balance billing.
- Annual Maximums: Most plans have a maximum dollar amount they will pay out per year. Once you hit this, you’re responsible for 100% of subsequent costs until the next benefit year.
- Deductibles: Some plans require you to pay a certain amount out-of-pocket before your insurance coverage begins.
Before proceeding with any major dental work, our team at Viva Dental Orangeville will always discuss the estimated costs with you, including your expected insurance coverage and your personal financial responsibility if you’re a senior citizen or earning less than CAD$30,000 annually.
Frequently Asked Questions About Dental Pre-Authorization
Q1: How long does dental pre-authorization take in Ontario?
A: For private insurance, it typically takes 1-3 weeks. For the Canadian Dental Care Plan (CDCP), current wait times can be longer, often several weeks to a month or more, especially for complex cases. We recommend planning well in advance for major treatments.
Q2: What documents are most important for pre-authorization?
A: The most crucial documents are recent diagnostic X-rays, a detailed treatment plan from your dentist, and comprehensive clinical notes explaining the necessity of the treatment. Photographs can also be very helpful.
Q3: Can I start my dental treatment without pre-authorization?
A: You can, but it’s generally not recommended for major work. Proceeding without pre-authorization means you are fully responsible for the entire cost if your insurance denies coverage or covers less than anticipated. It removes the financial clarity that pre-authorization provides.
Q4: What if my dentist isn’t participating in the CDCP, and I need pre-authorized work?
A: If your dentist is not participating in the CDCP, you will be responsible for the full cost of the treatment at the time of service. You can then submit a claim to the CDCP for reimbursement. However, the pre-authorization process still applies for major work. This means you would need to get the pre-authorization before proceeding if you want to ensure reimbursement eligibility from CDCP. Many dental clinics, including Viva Dental Orangeville, are actively participating in the CDCP to simplify this process for our patients.
Q5: How does pre-authorization for children’s dental work differ?
A: The process is largely the same for children, especially if they require major work like stainless steel crowns, pulpotomies (a form of root canal for baby teeth), or extensive orthodontic treatment. Many plans also have frequency limits on children’s treatments, so pre-authorization helps ensure coverage.
Your Path to a Healthy Smile, Clearly Understood
Understanding dental pre-authorization might seem daunting, but it’s a powerful tool for taking control of your dental health and finances. It allows you to approach major dental work with confidence, knowing what to expect from your insurance and what your personal investment will be. At Viva Dental Orangeville, under the leadership of Dr. Sahar Rakhshanfar, our commitment is to provide compassionate, high-quality care that you can trust. We are here to guide you through every step of your dental journey, from discussing treatment options and utilizing advanced dental technologies to navigating the complexities of insurance. We will work diligently to submit all necessary documentation for your pre-authorization requests, ensuring you receive the attention needed for optimal dental health.
Don’t let confusion about insurance delay essential dental care. We’re here to help make complex processes simple, so you can focus on achieving and maintaining a healthy, beautiful smile.